Are you ready for the coronavirus (COVID-19) pandemic that’s sweeping the world? Instead of enjoying a trip to San Antonio this morning for a medical meeting (which got canceled), my husband—as the chief medical officer of a local hospital— is acutely involved in preparing to meet the crisis which has come to Michigan. Two days ago (March 10, 2020) there were no confirmed cases in Michigan, although there were 760 cases confirmed in U.S. However, by 6:33 am on March 11, there were 1,039 confirmed cases throughout America and 119,476 world wide with 4,291 deaths. As of today, March 12th, there are 1,323 confirmed cases throughout America and 127,863 worldwide with 4,718 deaths. If you do the math, it’s shocking how fast this is traveling.
We also now have confirmed cases in Michigan. The schools have shut down in Grand Rapids, as they are where my kids live in California, Chicago, and New York. Belgium (where one of my sons lives) was leading the pack for new cases in Europe yesterday. I am amazed to read of people not taking this seriously. Come on, guys! Where’s your Boy Scout spirit? Semper paratus. Better safe than sorry! Don’t panic, but don’t ignore taking wise precautions, either, please!
Coronavirus is everywhere in the news, so this post may be too late to be particularly helpful, but just in case you haven’t done a lot of research yet, here’s the best up-to-the-moment coverage I have gleaned:
What are the symptoms of a COVID-19 (coronavirus) infection? Most commonly, it presents like flu and can include fever, tiredness and a dry cough, although other symptoms, such as achiness, pain, nasal congestion, runny nose, sore throat, or diarrhea are all possible. According to Dr. Martha Blum, MD PhD: “The most common presentation was one week prodrome of myaglias, malaise, cough, low grade fevers gradually leading to more severe trouble breathing in the second week of illness. It is an average of 8 days to development of dyspnea and average 9 days to onset of pneumonia/pneumonitis. It is not like Influenza, which has a classically sudden onset. Fever was not very prominent in several cases.”
How long does it take to determine if someone has COVID-19? According to the Center for Disease Control (CDC), “symptoms may appear anywhere between two to 14 days after exposure, with the average patient seeing onset at around five days.”
What should you do if you suspect you may be developing a COVID-19 infection ? Call (don’t visit) your doctor or your local health department. They can ask appropriate questions to determine whether on not you need to be tested. Obviously, you should not GO to the doctor’s office or health department directly, lest you expose others, but these health care locations can tell you where you would need to go for testing.
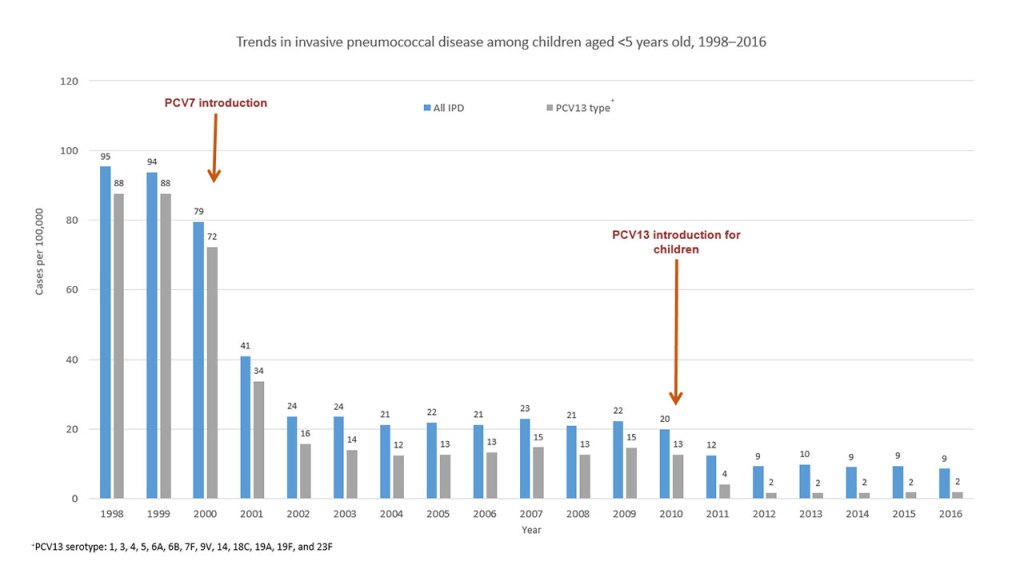
What can we do to prepare? Make sure all your immunizations are up to date. It’s still not too late to get your flu shot or a pneumonia vaccine if you are in the right age and risk group. Check with the Center for Disease Control and Prevention for specific guidelines (and other pertinent information concerning COVID-19): https://www.cdc.gov/
Beyond being properly immunized, all the sites I’ve studied say the #1. best advice is easy: limit your exposure as best you can and wash your hands with hot, soapy water for 20 seconds often and specifically after you’ve had contact with people in public places. Do NOT touch your face with your hands until after you’ve washed your hands carefully. If you have hand sanitizer as a second step (AFTER washing), that’s a plus, but most stores are out of hand sanitizer. You can also use rubbing alcohol as a disinfectant. I was able to find some this morning. Have a 14-30-day supply of food and medications on hand. I liked this list from USA Today (March 10, 2020 issue, and I quote):
•Food. Fresh fruits and vegetables will likely spoil over 14 days, so canned foods that have a long storage life and need little or no cooking are recommended. Meat products, fish or beans, soups, broths and stews, fruits and fruit juices, vegetables, canned (or powdered) milk, are among good supply choices recommended by the Texas A&M Agrilife Extension Disaster Education Network.
Frozen foods are an option, too. Other recommended foods are peanut butter, jelly, crackers, nuts, trail mix, dried fruits, granola bars, bouillon cubes, and staples like sugar, salt, pepper. (Keep in mind you may need to include some special foods for babies and family members on special diets, as well as pet foods.)
•Water and liquids. The Centers for Disease Control and Prevention suggests you have plenty of fluids on hand, such as bottled water and supply of fluids with electrolytes, such as Pedialyte or Gatorade. cdc.gov/healthywater/emergency/drinking/creating-storing-emergency-water-supply.html(opens in a new tab)
•Medicine. You will want to have a 14-day supply of any prescription medications for those in your home. You may also want over-the-counter pain relievers, antacids, cough and cold medicines, and vitamins.
•Supplies. Many homes already have a 14-day supply of most daily items on hand. But make sure you have toothpaste, toilet paper, feminine supplies, diapers, laundry detergent and disinfectant.
•Other items. Perhaps have some board games, cards, toys books, magazines and other fun items to keep the family occupied.
Okay, back to my editorializing: To keep abreast of what’s happening minute by minute around the world and in the U.S., you can access the Johns Hopkin Dashboard here:
https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
To track what’s happening in Michigan, here’s a link:
https://www.michigan.gov/coronavirus/
In case you think everybody’s overreacting, here’s a link that explains the importance of insulating ourselves and our communities as well as we possibly can. It can make a huge difference in the number of cases and the outcomes:
Below is a potpourri of various recommendations for immunizations, graphs and charts, a brief history of coronavirus, and other pertinent information that I’ve copy-and-pasted from websites, mostly the CDC.
When you are 65 years old, please get the PCV-13 first. Then you should get the Pneumovax 6-12 months afterwards. But if you’ve already had your Pneumovax, then get your PCV-13 one year later. If you are younger than 65, you might need a pneumonia vaccine if you have special conditions. Read more at the Center for Disease Control and Prevention: https://www.cdc.gov/vaccines/vpd/pneumo/public/index.html for more information
Shingles: https://www.cdc.gov/shingles/vaccination.html “Two shingles vaccines are licensed and recommended in the United States. Zoster vaccine live (ZVL, Zostavax) has been used since 2006, and recombinant zoster vaccine (RZV, Shingrix), has been used since 2017, and is recommended as the preferred shingles vaccine.” My vaccine made both my sister and me quite ill briefly, and it does have transiet flu-like side effects for more than half the population, so choose a day when you don’t have much scheduled. We chose a Friday afternoon with a clear weekend.
Interim guidance is available at https://www.cdc.gov/coronavirus/index.html. As more is learned about this virus and the outbreak, CDC will rapidly incorporate new knowledge into guidance for action.
For historical perspective from the CDC: “An outbreak of coronavirus disease 2019 (COVID-19) caused by the 2019 novel coronavirus (SARS-CoV-2) began in Wuhan, Hubei Province, China in December 2019, and has spread throughout China and to 31 other countries and territories, including the United States (1). As of February 23, 2020, there were 76,936 reported cases in mainland China and 1,875 cases in locations outside mainland China (1). There have been 2,462 associated deaths worldwide; no deaths have been reported in the United States. Fourteen cases have been diagnosed in the United States, and an additional 39 cases have occurred among repatriated persons from high-risk settings, for a current total of 53 cases within the United States. This report summarizes the aggressive measures (2,3) that CDC, state and local health departments, multiple other federal agencies, and other partners are implementing to slow and try to contain transmission of COVID-19 in the United States. These measures require the identification of cases and contacts of persons with COVID-19 in the United States and the recommended assessment, monitoring, and care of travelers arriving from areas with substantial COVID-19 transmission. Although these measures might not prevent widespread transmission of the virus in the United States, they are being implemented to 1) slow the spread of illness; 2) provide time to better prepare state and local health departments, health care systems, businesses, educational organizations, and the general public in the event that widespread transmission occurs; and 3) better characterize COVID-19 to guide public health recommendations and the development and deployment of medical countermeasures, including diagnostics, therapeutics, and vaccines. U.S. public health authorities are monitoring the situation closely, and CDC is coordinating efforts with the World Health Organization (WHO) and other global partners. Interim guidance is available at https://www.cdc.gov/coronavirus/index.html. As more is learned about this novel virus and this outbreak, CDC will rapidly incorporate new knowledge into guidance for action by CDC, state and local health departments, health care providers, and communities.
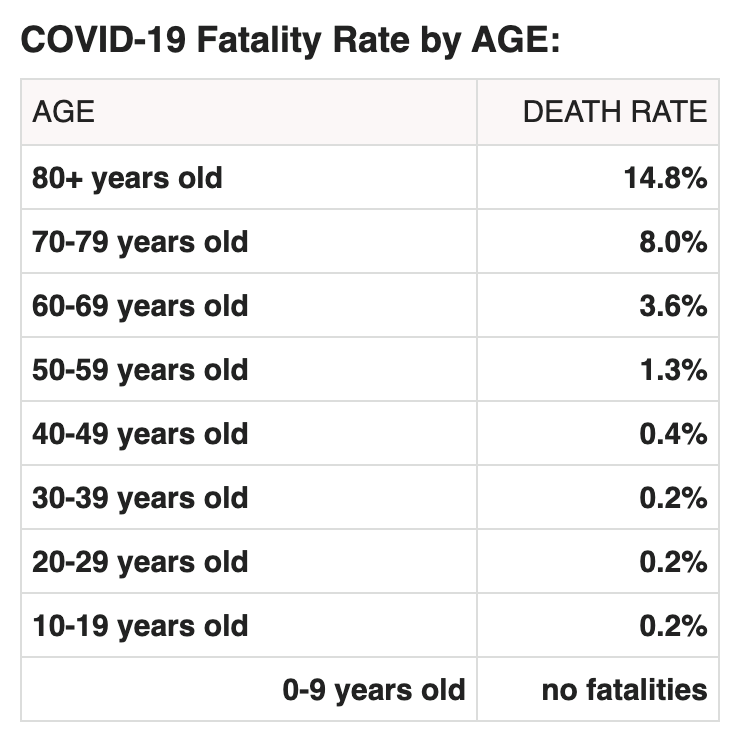
“Person-to-person spread of COVID-19 appears to occur mainly by respiratory transmission. How easily the virus is transmitted between persons is currently unclear. Signs and symptoms of COVID-19 include fever, cough, and shortness of breath (4). Based on the incubation period of illness for Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) coronaviruses, as well as observational data from reports of travel-related COVID-19, CDC estimates that symptoms of COVID-19 occur within 2–14 days after exposure. Preliminary data suggest that older adults and persons with underlying health conditions or compromised immune systems might be at greater risk for severe illness from this virus (5).
Information for travelers: CDC.gov/Travel
https://www.cdc.gov/coronavirus/2019-ncov/about/prevention-treatment.html
“There is currently no vaccine to prevent coronavirus disease 2019 (COVID-19). The best way to prevent illness is to avoid being exposed to this virus. However, as a reminder, CDC always recommends everyday preventive actions to help prevent the spread of respiratory diseases, including:
- Avoid close contact with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe.
- Follow CDC’s recommendations for using a facemask.
- CDC does not recommend that people who are well wear a facemask to protect themselves from respiratory diseases, including COVID-19.
- Facemasks should be used by people who show symptoms of COVID-19 to help prevent the spread of the disease to others. The use of facemasks is also crucial for health workers and people who are taking care of someone in close settings (at home or in a health care facility).
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating; and after blowing your nose, coughing, or sneezing.
- If soap and water are not readily available, use an alcohol-based hand sanitizer with at least 60% alcohol. Always wash hands with soap and water if hands are visibly dirty.
“There is no specific antiviral treatment recommended for COVID-19. People with COVID-19 should receive supportive care to help relieve symptoms. For severe cases, treatment should include care to support vital organ functions.”
Why is it so much more dangerous for elderly people? According to Bruce Aylward (who leads the World Health Organization’s infectious disease response team), “These people are dying of an inflammatory process in their lungs. It’s not an infectious process, like a bacterial or viral infection. It’s inflammatory, like we see with SARS. We’re not sure of the mechanism. We do know the proportion of people who die who had cancer was half compared to hypertension and cardiovascular disease. Diabetes is a little bit lower than those two, and cancer lower again.
Italy is currently locked down. In China, the cases are diminishing. In America, the confirmed cases are growing rapidly!
After all is said and done, I would like to remind people to prepare, but not panic! Prepare, watch, and pray: “The horse is prepared against the day of battle: but safety is of the Lord ” (Proverbs 21:31). Our world, our times, and our lives are ultimately in the hands of the One who has created us. As Solomon taught, “Let us hear the conclusion of the whole matter: Fear God, and keep his commandments: for this is the whole duty of man. For God shall bring every work into judgment, with every secret thing, whether it be good, or whether it be evil” (Ecclesiastes 12:13-14). I am totally convinced that this current plague is intended by God for our good, to bring us all to the foot of the cross, where we can find rest and peace for our souls—and eternal life through faith in Christ—despite the present crisis. “God is our refuge and strength, a very present help in trouble. Therefore will not we fear, though the earth be removed, and though the mountains be carried into the midst of the sea” (Psalm 46:1-2).
Please feel free to write a response, ask any questions, or request me to pray for you specifically.
